Abstract

Introduction
Women with inherited bleeding disorders (IBD) are at increased risk of peripartum bleeding complications. The aim of our study was to assess our institutional outcomes of management of women with IBD during pregnancy and the peripartum period.
Methods
Eligible patients included women with IBD followed at the Mayo Clinic, Rochester Hemophilia Treatment Center and were followed at our institution for antenatal and peripartum care. Patients were excluded if detailed delivery outcomes were unavailable in the electronic medical record (EMR). If delivery was not in our institution but all records were available to review in EMR the pregnancy was included in analysis if our group was primarily involved in providing management recommendations. The EMR was retrospectively reviewed and details regarding factor usage, delivery method and outcome, analgesia, and post-partum hemorrhage (PPH) were recorded. Thrombotic complications 6 weeks post-partum was also recorded.
Results
73 pregnancies in 46 unique patients met our inclusion criteria for this study. Distribution of underlying IBD in the 73 pregnancies was as follows: 50% type 1 VWD (n=37), 15% (n=11) hemophilia A carrier, baseline (bl) fVIII 46 (21-88)%.), and 13.7% (n=10) hemophilia B carrier (bl fIX 43 (23-69)% . In the remaining pregnancies, underlying IBD included type 2 VWD (n=6), type 3 VWD (n=1), VWF multimer abnormality (n=2) , factor XI deficiency (n=2, bl fXI: 44%), factor VII deficiency (n=2, bl fVII 37%) and factor V deficiency (n=2, bl fV 11%). Surprisingly, at the time of 24 deliveries, the patient's bleeding disorder (type 1 VWD, n=15) had not yet been diagnosed.
In 56 % of pregnancies (n=41), a hematology delivery plan was in place prior to admission for delivery. Of 30 delivery inductions, 11 were performed due to IBD. There were 46 vaginal deliveries, 25 C-sections, and 2 dilation and curettage (D&C). Two C-sections were recommended due to IBD (hemophilia B and type 2 VWD). In 37/46 of vaginal deliveries neuraxial anesthesia was used with no complications noted.
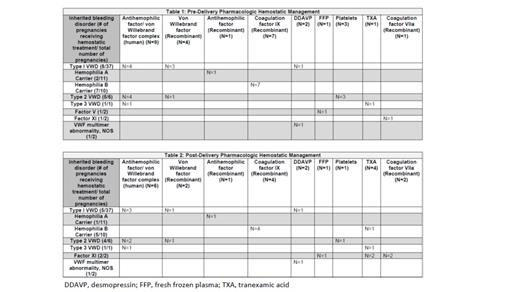
26 deliveries were performed under the cover of hemostatic pharmacologic agents (Table one). Due to naturally increasing levels of VWF during the peripartum period, only 8/37 (21.6 %) pregnancies in those with type 1 VWD required hemostatic treatment.
61/73 pregnancies were at least at early term (>37 weeks) and all resulted in live birth. Of the remaining pregnancies (n=12), 5 resulted in a nonviable fetus. In one pregnancy, fetal demise was due to termination of pregnancy due to type III VWD and recent lymphoma in the mother.
Pharmacologic hemostatic agents were used in 19 pregnancies in the post-partum period (Table 2). 10 pregnancies (6 vaginal), met American College of Gynecology criteria for early PPH. Underlying IBD for pregnancies with PPH included (type 1 VWD: n=7,hemophilia A carrier (n=1), type II VWD (n=1), factor VII deficiency (n=1). 4 of these had received pharmacologic hemostatic treatment prior to delivery. Primary management of PPH involved uterine intervention (ie. Massage and uterotonic agents). In three pregnancies, a D&C was required (one due to stillborn birth and two due to retained placenta). One case of PPH was due to placental abruption. Additional pharmacologic hemostatic management was utilized in 4 deliveries where PPH was noted. Red blood cell transfusions were needed in 3 pregnancies due to PPH. There were no thrombotic complication up to 6 weeks post-partum.
Conclusion
Though rates of early PPH were >10% in our cohort, most causes of PPH were unrelated to the underlying IBD. Although the current study is limited due to lack of many patients with type II and III VWD, results demonstrate that bleeding risk during delivery due to the IBD is low when patients are evaluated and managed with the use of a multidisciplinary care team.
Pruthi: CSL Behring: Honoraria; Merck: Honoraria; HEMA Biologics: Honoraria; Bayer Healthcare AG: Honoraria; Genentech: Honoraria; Instrumentation Laboratory: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal